Dr. Victoria Vardell Publishes "Influence of Racial and Ethnic Identity On Overall Survival in Chronic Lymphocytic Leukemia Patients"
Dr. Victoria Vardell was the first author on "Influence of Racial and Ethnic Identity On Overall Survival in Chronic Lymphocytic Leukemia (CCL) Patients", a study which seeks to understand the impact of race on the survival of Lymphocytic Leukemia.

This report examined the largest cohort of underrepresented racial and ethnic minority CLL patients. Currently, CCL is the most prevalent adult leukemia in the United States and an estimated 87-89% of patients are White. Previous studies suggest racial and ethnic minority CLL patients have reduced survival rates compared with White patients.
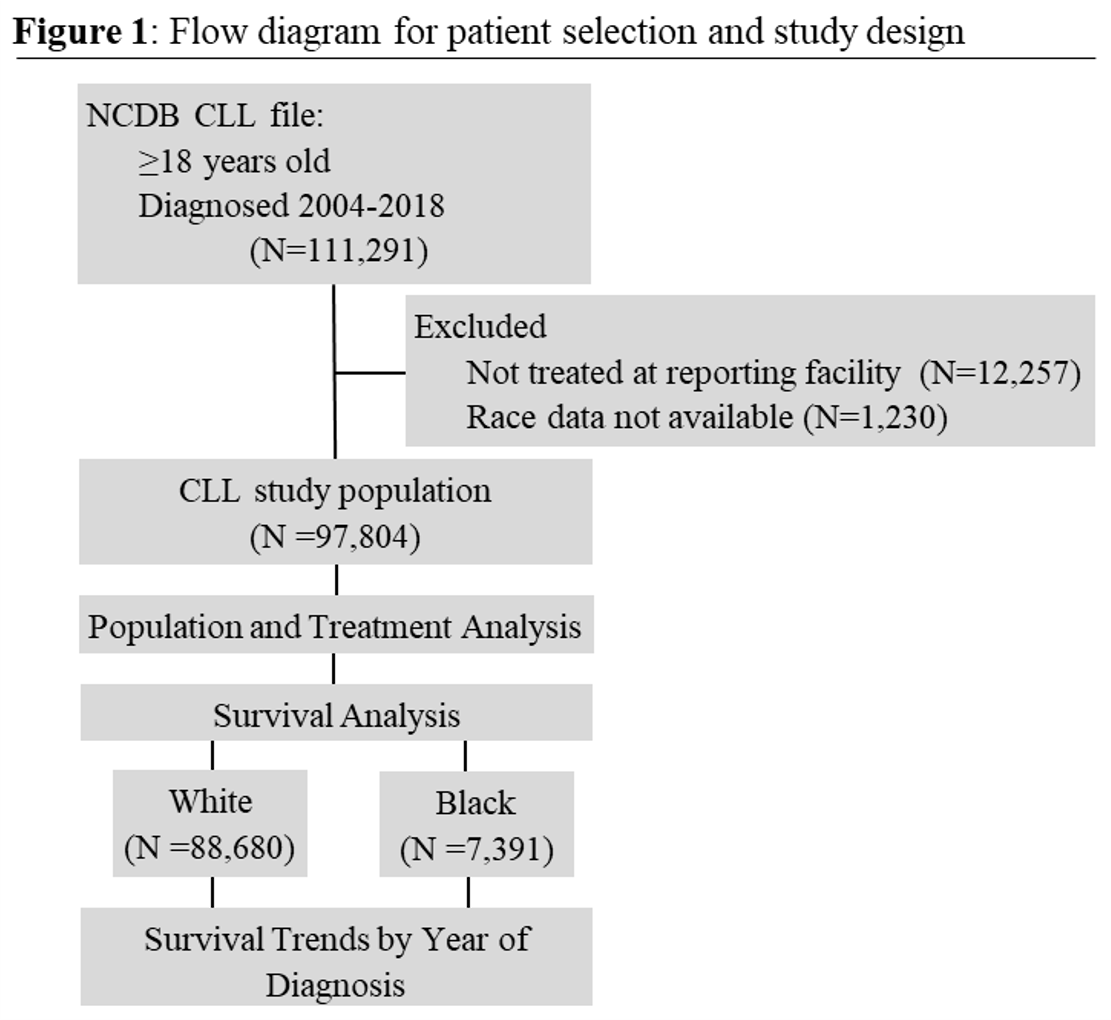
The study used the National Cancer Database for Chronic Lymphocytic Leukemia to examine characteristics of each population; then completed a survival analysis to compare how the survival rate has changed between groups over time.
When examined, the data showed that Black and other racial minority patients are diagnosed at a younger age than White patients.
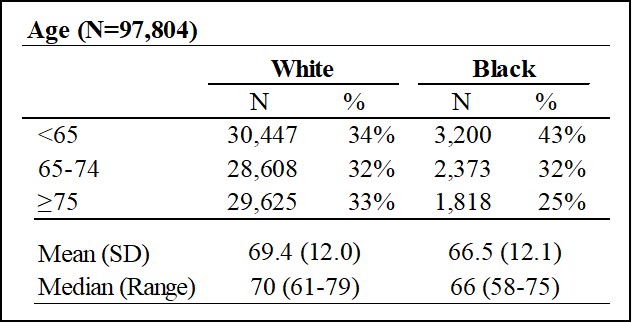
In addition, Black patients had a higher comorbidity burden at diagnosis than White patients.
Overall, Black patients, when compared to White patients, were more likely to:
- Be female (42.8% vs 39.3%)
- Be uninsured (6.6% vs 2.1%)
- Be insured by Medicaid (9.9% vs 3.4%)
- Reside in low income areas (47.7% vs 13.1%)
- Reside in areas with low high school graduation rates (41.3% vs 14.3%)
- Receive systemic CLL directed therapy at diagnosis.
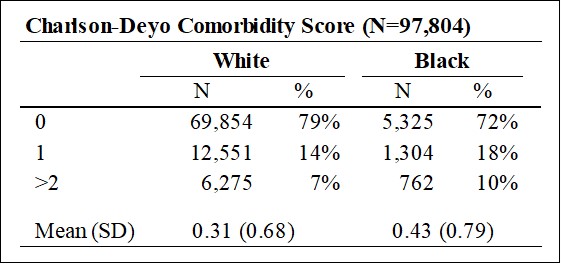
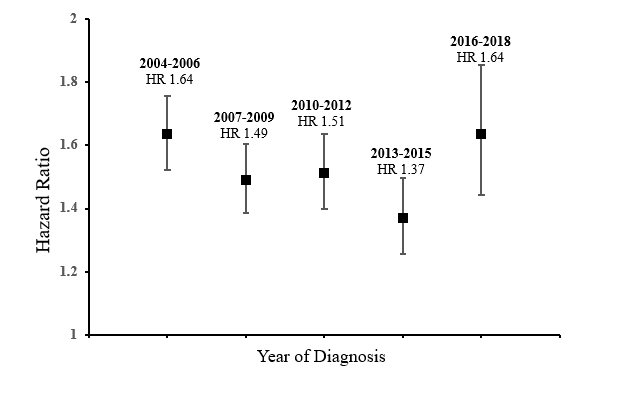
Following the study of racial and ethnic characteristics, the survival analysis was performed. With a median follow up of 4.3 years, the median OS for all CLL patients was 9 years (95% confidence, 8.9-9.1 years). Black patients had a shorter median OS of 7 years (95% confidence, 6.7-7.3 years). On multivariate Cox regression, adjusted for age and Charlson-Deyo comorbidity score, Black patients had significantly increased risk of death compared to White patients [HR 1.51 (95% CI 1.46-1.57, p<0.001)].
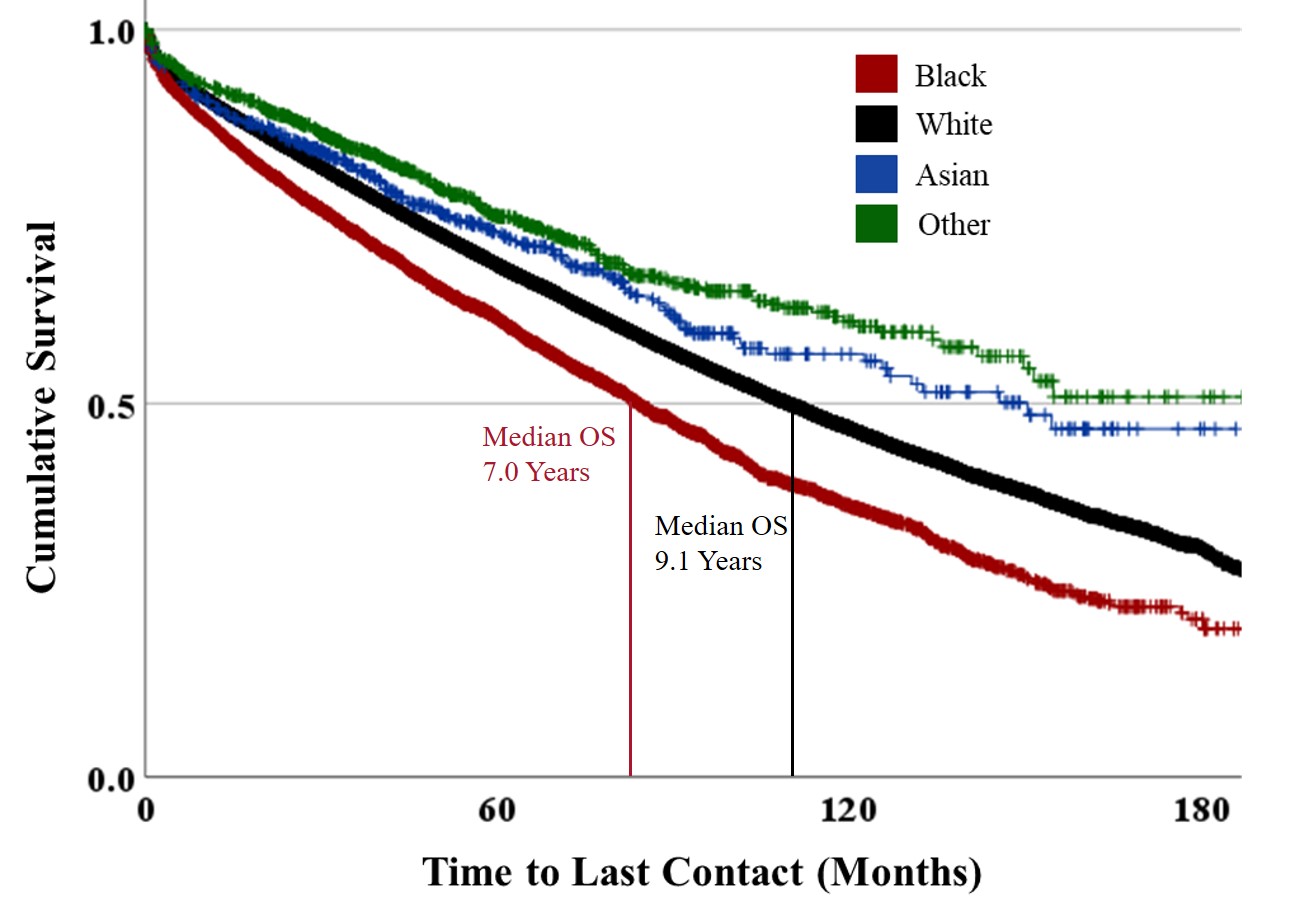
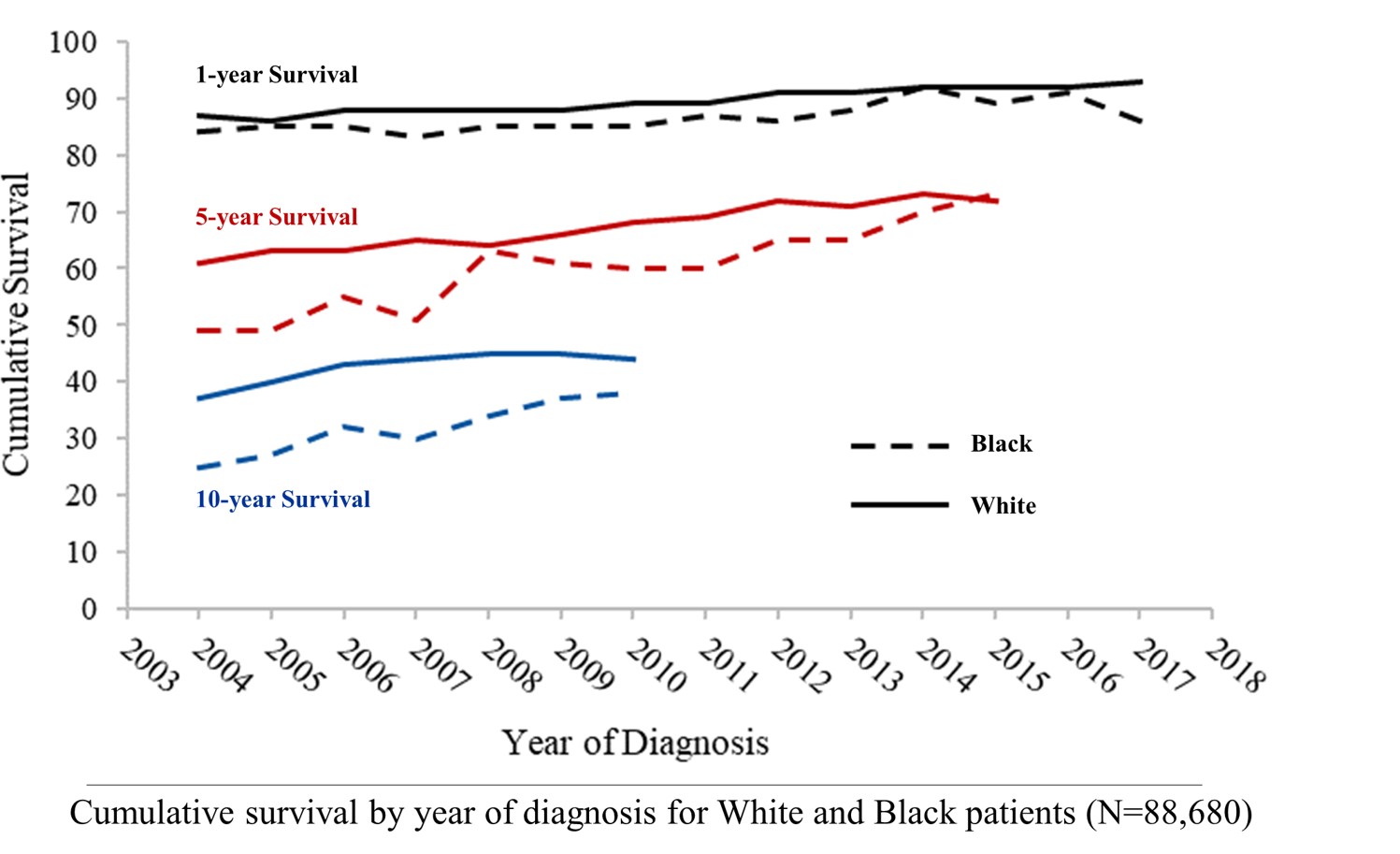
Then an attempt was made to examine how the relative disparity between White and Black patients has change with time. This graph shows the 1, 5, and 10 year proportional survival by year of diagnosis for both White and Black patients. It appears to improve over time (especially at 5 and 10 years) for both cohorts, and appears there may be improvement; however this is unadjusted and difficult to determine significance of the trends.
Finally, a multivariate cox regression was perforated (again adjusting for age and comorbidity burden) by time period of diagnosis to compare the risk of all cause mortality for Black patients compared to the White population. As demonstrated on the forest plot below, no significate change over time was observed.
In summary, this report is the largest study to date (97,804 patients) on the characteristics and outcomes of CLL patients from underrepresented races and ethnicities. We found:
- Black and other racial minority patients present at a significantly younger age than White patients
- Black patients have a significant increase in comorbid diagnosis
- Black and other racial minority patients have significantly increased socioeconomic disadvantage
- Black patients are more likely to receive treatment at diagnosis (this may indicate more advanced disease at diagnosis)
Black patients have significantly reduced survival compared to White patients (and those of other races) in the era of targeted oral CLL therapies.
- Disparity persisted when adjusted for age and comorbidity score
- There is a trend towards improvement in the overall survival disparity, particularly in 5 year OS, in the last 15 years
These disparities do not appear to have improved since 2004. Factors that may contribute to that include:
- Higher rates of comorbid diagnoses
- Socioeconomic disparity
- Low income
- Underinsurance
- Advanced or higher molecular risk disease at diagnosis
Victoria A. Vardell, MD, Daniel A. Ermann, MD, Lindsey Fitzgerald, MD, Harsh Shah, DO, Boyu Hu, MD, Deborah M. Stephens, DO
Internal Medicine, University of Utah, Salt Lake City, UT; Division of Hematology and Hematologic Malignancies, Huntsman Cancer Institute, University of Utah, Salt Lake City, UT